On Aug. 8, 2019, Florida’s Surgeon General Dr. Scott Rivkees declared a public health emergency regarding Hepatitis A. This declaration is in response to the significant increase in confirmed Hepatitis A and cases and is designed to help spread awareness of risk and prevention among the public. FRLA applauds the efforts of Dr. Rivkee to keep Floridians and our guests healthy, and we have actively partnered with the Florida Department of Health (FDOH) to educate hospitality workers. While those who work in hotels and restaurants are at no higher risk than the general population, the Association recognized our opportunity to reach a significant number of Floridians with the FDOH message because we represent the state’s largest industry.
Since partnering with FDOH, FRLA Education and Training, Membership, and Communications teams have worked to educate the hospitality industry about Hepatitis A and how best to prevent the spread of this disease. We have shared messaging via email, on social media, and at local events in areas most impacted by Hepatitis A.
Frequently Asked Questions
What is Hepatitis A and how is it spread?
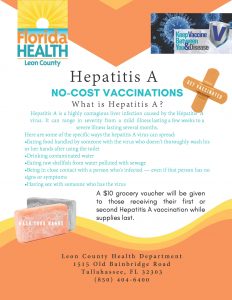
Hepatitis A is a highly contagious liver infection caused by the Hepatitis A virus (HAV), usually spread through close personal contact, food, water, or any object contaminated with HAV from the feces of an infected person.
What are the symptoms and duration of Hepatitis A?
Hepatitis A is a self-limited disease that does not result in chronic infection. Common symptoms in adults nclude yellowing skin, fever, diarrhea, stomach pain, fatigue, and loss of appetite. Generally, symptoms appear two to six weeks after exposure and last less than two months, although some people may be ill for as long as six months.
What is the difference between Hepatitis A, B, and C?
According to the U.S. Centers for Disease Control and Prevention (CDC), each disease may cause similar symptoms, but they spread in different ways and can affect the liver differently. HAV is usually a short-term infection while Hepatitis B and C may begin as short-term infections but persist and cause lifelong (chronic) infection.
Is Hepatitis A increasing in Florida?
Yes. The number of reported cases of Hepatitis A in Florida are significantly higher than preceding years. However, this increase is not isolated to Florida. In fact, the CDC reports that the current national outbreak was identified in 2016 and includes 25 states.
Why did the Florida Surgeon General declare a public health emergency for Hepatitis A?
Dr. Rivkees made this declaration to raise awareness of the disease and ways to limit its spread.
Who is most at risk for Hepatitis A?
According to the Florida Surgeon General, those most at risk are:
- Individuals experiencing homelessness
- Those who use intravenous drugs
- Those who use non-intravenous illicit drugs
- Men who have sex with men
- Individuals diagnosed with underlying liver disease
- Individuals in an emergency room or other acute care setting after being administered an opioid antagonist such as naloxone
- Those working outside a health care setting with people experiencing homelessness or people who use intravenous drugs
- Individuals over the age of 60 with a serious underlying medical condition, as determined by their health care providers, in critically impacted counties
- First responders
What can food service operators do to reduce the spread of Hepatitis A?
Operators can and should:
- Ensure frequent and proper food safety training for all food workers and their supervisors. You can find training here.
- Communicate the risk to employees. Use alley rallies, line-ups, or similar staff mini-meetings to frequently and continually discuss Hepatitis A symptoms, danger, and risk education.
- Observe and enforce proper hand-washing technique.
- Eliminate bare hand contact with ready-to-eat foods.
- Exclude and restrict ill employees from working around food as required by the US FDA Food Code.
- Actively observe employees for symptoms, noticing if employees show signs or symptoms of Hepatitis A or other illness. Implement an Employee Health Agreement and actively manage it.
- Implement a daily surface-sanitizing procedure that includes all high-touch areas and objects not sanitized as part of regular operations. For example, menus, door knobs and handles, and POS screens.
- Encourage voluntary Hepatitis A vaccination for high-risk persons.
Hyper-vigilant, active managerial control of these factors and all food safety best practices are essential to reducing Hepatitis A and food-borne illness risks.
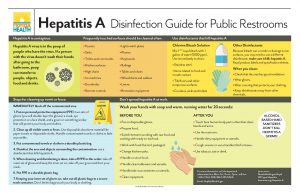
What are proper hand-washing techniques?
- Use 100° F hot water, soap, and sufficient friction for at least 10-15 seconds according to the 2017 Food Code.
- Wash hands before, during, and after preparing food; before eating food; before and after caring for someone who is sick; before and after treating a cut or wound; after using the toilet; after changing diapers or cleaning a child who has used the toilet; after blowing your nose, coughing, or sneezing.
- Alcohol-based hand sanitizers do not kill the Hepatitis A virus.
Are vaccines available to prevent Hepatitis A?
Yes. Talk with your primary care provider or a medical professional about options. Many local county health departments in Florida are offering free or reduced-price Hepatitis A vaccinations. The full vaccine is a two-part series with the second shot administered approximately six months after the first. However, if exposure is suspected, vaccination can still prevent Hepatitis A. The CDC reports that one dose of single-antigen Hepatitis A vaccine provides up to 95% protection in healthy individuals for up to 11 years.
Where can I find more information about Hepatitis A?
The CDC, the Florida Department of Health, and the National Restaurant Association all have resources specifically for Hepatitis A.
What should a food service operator do if an employee tests positive for Hepatitis A?
If an employee contracts Hepatitis A, quick reaction is critical in reducing risk to patrons and other employees. Upon learning of a positive diagnosis, operators should immediately:
- Contact the local county health department and follow their directions.
- Re-train all food employees on hand-washing, bare hand contact, and employee health policies.
- Implement a daily surface-sanitizing procedure that includes all high-touch areas and objects not sanitized as part of regular operations – menus, door handles and knobs, cell phones, telephones, POS screens, etc.
- Prepare for media attention and consider consulting professionals experienced in crisis communications.
- Contact FRLA so that we can provide you support.